Philip Wenzel
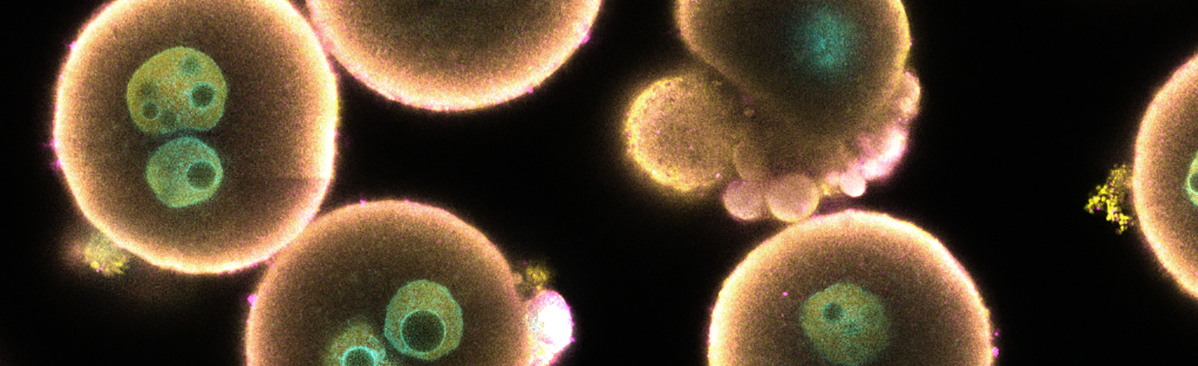
Vascular Inflammation
Vascular inflammation leads to endothelial dysfunction and is an important contributing factor in the pathophysiology of ageing and age-related cardiovascular diseases such as arterial hypertension, coronary artery disease and heart failure. Importantly, vascular inflammation pathways have great potential in the development of new therapies: there are many potentially druggable targets that could benefit patients with myocardial infarction, venous thromboembolism and ischemia-reperfusion damage, as well as chronic inflammatory diseases such as psoriasis, and even stress and noise exposure.
In our group, we are particularly concerned with the importance of CD11b+ myeloid cells, especially monocytes/macrophages. We are also interested in the influence of coagulation factors of the contact phase system, thrombin amplification and the tissue factor system in vascular inflammation.
Our research interests are:
- The role of inflammatory myelomonocytic cells in activation of the renin-angiotensin-aldosterone system
- The interaction of coagulation factors, leukocytes and platelets in vascular dysfunction, ischemic and nonischemic heart failure and atherothrombosis
- The systemic role of vascular inflammation in age-related decline of organ function
Positions held
- Since 2022: Extraordinary Professor, Johannes Gutenberg University, Mainz
- Since 2016: Deputy Director, Center for Cardiology, Cardiology I, University Medical Center (UMC), Mainz
- 2017: Principal Investigator, German Centre for Cardiovascular Research (DZHK)
- 2016 - 2022: Professor (W2) of Vascular Inflammation, Center for Cardiology, Cardiology I and Center for Thrombosis and Hemostasis (CTH), University Medical Center (UMC), Mainz
- 2011 - 2014: Junior Research Group Leader, Centre for Thrombosis and Hemostasis (CTH), University Medical Center (UMC), Mainz
- 2003 - 2011: Residency in Internal Medicine and Cardiology, University Medical Center Hamburg Eppendorf, University Medical Center (UMC), Mainz
Education
2010: Habilitation, University Medical Center (UMC), Mainz
2003: MD-Thesis, Institute for Sports Medicine, University Hamburg
1995 - 2002: Medical School, Friedrich Alexander-University, Erlangen-Nürnberg University Hamburg
Selected publications by Philip Wenzel
Garlapati V, Molitor M, Michna T, Harms GS, Finger S, Jung R, Lagrange J, Efentakis P, Wild J, Knorr M, Karbach S, Wild S, Vujacic-Mirski K, Münzel T, Daiber A, Brandt M, Gori T, Milting H, Tenzer S, Ruf W and Wenzel P (2022) Targeting myeloid cell coagulation signaling blocks MAP kinase/TGF-β1 driven fibrotic remodeling in ischemic heart failure. J Clin Invest, 133:e156436 Link
Efentakis P, Molitor M, Kossmann S, Bochenek ML, Wild J, Lagrange J, Finger S, Jung R, Karbach S, Schäfer K, Schulz A, Wild P, Münzel T and Wenzel P (2022) Tubulin-folding cofactor E deficiency promotes vascular dysfunction by increased endoplasmic reticulum stress. Eur Heart J, 43:488–500 Link
Kossmann S*, Lagrange J*, Jackel S, Jurk K, Ehlken M, Schonfelder T, Weihert Y, Knorr M, Brandt M, Xia N, Li H, Daiber A, Oelze M, Reinhardt C, Lackner K, Gruber A, Monia B, Karbach SH, Walter U, Ruggeri ZM, Renne T, Ruf W, Münzel T and Wenzel P (2017) Platelet-localized FXI promotes a vascular coagulation-inflammatory circuit in arterial hypertension. Sci Transl Med, 9:eaah4923 (*indicates joint contribution) Link
Wenzel P, Rossmann H*, Muller C*, Kossmann S*, Oelze M, Schulz A, Arnold N, Simsek C, Lagrange J, Klemz R, Schonfelder T, Brandt M, Karbach SH, Knorr M, Finger S, Neukirch C, Hauser F, Beutel ME, Kroller-Schon S, Schulz E, Schnabel RB, Lackner K, Wild PS, Zeller T, Daiber A, Blankenberg S and Münzel T (2015) Heme oxygenase-1 suppresses a pro-inflammatory phenotype in monocytes and determines endothelial function and arterial hypertension in mice and humans. Eur Heart J, 36:3437–3446 (*indicates joint contribution) Link
Wenzel P*, Knorr M*, Kossmann S, Stratmann J, Hausding M, Schuhmacher S, Karbach SH, Schwenk M, Yogev N, Schulz E, Oelze M, Grabbe S, Jonuleit H, Becker C, Daiber A, Waisman A and Münzel T (2011) Lysozyme M-positive monocytes mediate angiotensin II-induced arterial hypertension and vascular dysfunction. Circulation, 124:1370–1381 (*indicates joint contribution) Link